Good Doctor. Hot Infusion | Reprint 1: Clinical or laboratory research progress -- Small bowel transplantation for pseudomyxoma peritonei
Pseudomyxoma peritonei (PMP) is a rare clinical syndrome characterized by mucinous ascites, peritoneal implants, and the formation of omental cakes. The vast majority of PMP originates from perforation of appendiceal mucinous tumors, while a minority originates from other organs such as the ovaries, umbilical cord, colon, and pancreas. Perforation of mucinous tumors leads to the shedding of mucin and mucin-producing epithelial cells into the peritoneal cavity. Through redistribution, it spreads sequentially to the right paracolic gutter, right subphrenic space, left subphrenic space (including the spleen), greater omentum, and pelvic floor (including the ovaries and uterus in females) [Carr NJ et al., Am J Surg Pathol. 2016]. PMP usually progresses slowly and rarely metastasizes to lymph nodes or distant sites.
2025-04-29
Small bowel transplantation for pseudomyxoma peritonei
By Nada Ayoub*, Srikanth Reddy^ and Tom Cecil*
*Peritoneal Malignancy Institute, Hampshire Hospitals NHS Foundation Trust, Basingstoke, UK
^Oxford Transplant Centre, Oxford University Hospitals NHS Foundation Trust, Oxford, UK
Foreword
Pseudomyxoma peritonei is a rare clinical syndrome characterized by mucinous ascites, peritoneal implants, and the formation of omental cakes. The vast majority of pseudomyxoma peritonei originates from the perforation of appendiceal mucinous tumors, while a minority originates from other organs such as the ovaries, umbilical cord, colon, and pancreas. Perforation of mucinous tumors leads to the shedding of mucin and mucin-producing epithelial cells into the abdominal cavity. Through redistribution, it spreads sequentially to the right paracolic gutter, right subphrenic space, left subphrenic space (including the spleen), greater omentum, and pelvic floor (including the ovaries and uterus in women) [Carr NJ et al., Am J Surg Pathol. 2016]. Pseudomyxoma peritonei usually progresses slowly and rarely metastasizes to lymph nodes or distant sites.
Currently, cytoreductive surgery plus intraperitoneal hyperthermic chemotherapy is the standard treatment for pseudomyxoma peritonei. This involves the combined resection of organs and peritoneum to remove all visible tumors as much as possible, followed by intraoperative intraperitoneal hyperthermic chemotherapy. The hyperthermic chemotherapy drug usually used is mitomycin C. Classic cytoreductive surgery includes parietal peritoneum resection, greater and lesser omentum resection, appendectomy, or right hemicolectomy (applicable to high-grade appendiceal mucinous tumors, goblet cell carcinomas, or right hemicolon mucinous adenocarcinomas). Female patients usually undergo bilateral adnexectomy and hysterectomy. Depending on the extent of tumor involvement, selective resection of the right and left diaphragmatic peritoneum, pelvic peritoneum, spleen, gastrointestinal tract, and hepatic capsule is performed [Sugarbaker PH. Surg Oncol Clin N Am 2003]. Up to 80% of patients with pseudomyxoma peritonei can achieve complete cytoreduction.
However, even after complete cytoreductive surgery and intraperitoneal hyperthermic chemotherapy, 22% to 44% of patients experience recurrence, and some patients cannot undergo cytoreductive surgery again. In some patients, due to extensive small bowel involvement, complete tumor resection cannot be achieved, and only maximal traditional debulking surgery can be performed. The inevitable progression of residual lesions is unavoidable [Ahmadi N et al., Ann Surg Oncol. 2021].
Due to extensive small bowel involvement, patients gradually experience abdominal distension and malnutrition, requiring parenteral nutrition support. Abdominal wall defects and intestinal fistulas are common at this stage of the disease, making effective relief of symptoms increasingly difficult or even impossible, causing significant patient suffering. Inspired by the story of patient Steve Prescott [One in a million: My story Vertical Editions ISBN-13 978-1904091844], based on the clinical characteristics of this stage of the disease and the relatively slow progression of pseudomyxoma peritonei, doctors began to seek surgical solutions. Ultimately, modified multi-organ transplantation/small bowel transplantation may become a surgical option for treating and alleviating the condition of such patients, and is expected to improve patient survival rates and quality of life.
Small bowel transplantation
Currently, small bowel transplantation has become a mature treatment option for an increasing number of diseases. However, compared to other solid organ transplants (such as kidney and liver transplants), small bowel transplantation has a higher incidence of complications and lower patient survival rates.
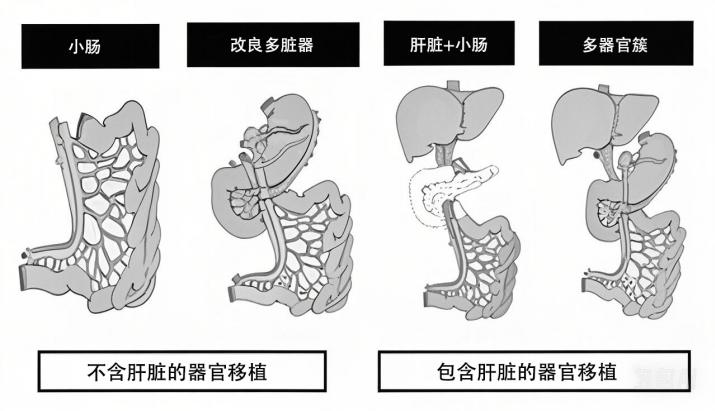
The following figure outlines different small bowel transplantation options. The complexity of the graft determines the surgical risk and outcome.
Small bowel transplantation for pseudomyxoma peritonei
The pseudomyxoma peritonei team at the Basingstoke Peritoneal Malignancy Institute collaborated with the transplant team at Oxford University to conduct a small bowel transplantation project for patients with end-stage pseudomyxoma peritonei. This article will discuss 15 cases of simple small bowel transplantation or modified multi-organ transplantation from the aspects of surgical methods, lessons learned, and clinical outcomes.
Inclusion criteria for multi-organ transplantation/small bowel transplantation
1. Diffuse pseudomyxoma peritonei with a peritoneal cancer index of 30-39, small bowel involvement, and no effective chemotherapy or conventional surgical options.
2. According to the pathological classification criteria of the Peritoneal Surface Oncology Group International (PSOGI), it belongs to low-grade lesions or slowly progressing high-grade lesions.
3. Malnutrition, requiring or about to require parenteral nutrition support.
Exclusion criteria for multi-organ transplantation/small bowel transplantation
1. Presence of distant metastases.
2. Severe cardiac or other organ dysfunction that prevents the patient from tolerating transplantation surgery.
3. Severe condition where transplantation surgery may not provide relief, with a short life expectancy.
4. Poor patient compliance, non-compliance with medical advice posing a risk to the transplanted organ.
5. Patient does not accept the potential complications of using immunosuppressant drugs.
6. Acquired immunodeficiency syndrome (AIDS) (diagnosed according to CDC standards: CD4+ cell count ≤200/mm³), unless the following criteria are met:
a. CD4+ cell count > 200/mm³ and duration exceeding six months.
b. Human immunodeficiency virus type 1 (HIV-1) ribonucleic acid (RNA) test negative.
c. Receiving stable antiretroviral therapy for more than three months.
d. No other AIDS-related complications (opportunistic infections such as aspergillosis, tuberculosis, coccidioidomycosis, drug-resistant fungal infections; Kaposi's sarcoma or other tumors).
e. Meets all other criteria for small bowel transplantation or multivisceral transplantation.
Donor Surgery
A modified multivisceral allograft, including the stomach, duodenum-pancreas, small bowel, and right hemicolon, was harvested from all donors. In addition, a full-thickness abdominal wall with its inferior epigastric vessels was harvested when needed.
Recipient Surgery
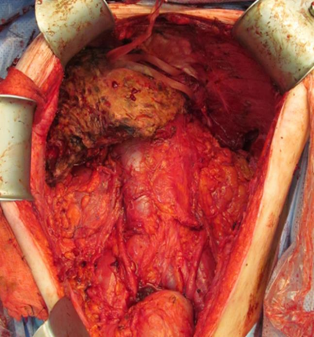
Once donor organ suitability was confirmed, recipient surgery commenced immediately, taking advantage of the typically lengthy procurement process to excise the involved bowel. Approximately half of the patients required resection of the duodenum, pancreas, stomach, small bowel, and colon due to extensive tumor infiltration.
The graft was selected based on the extent of abdominal organ involvement, with the principle of transplanting the minimum amount of donor tissue necessary while ensuring effective tumor resection. Some patients with less upper abdominal tumor recurrence could retain their stomach, duodenum, and pancreas. Although complete tumor cell ablation was pursued, a small amount of residual tumor was sometimes left for safety reasons, especially in the hepatoduodenal or diaphragmatic areas. In some cases, high-power electrocautery was used to ablate liver surface tumors by resecting the liver capsule.
For isolated bowel transplantation, vascular reconstruction involved anastomosis of the donor superior mesenteric vessels to the recipient. In multivisceral transplantation, a segment of the donor thoracic aorta was used as an infrarenal aortic bridge to the recipient, anastomosed to a Carrel patch containing the donor superior mesenteric artery and celiac trunk, establishing venous outflow via anastomosis to the recipient portal vein.
|
Pseudomyxoma Peritonei Resection Specimen |
Pseudomyxoma Peritonei Resection Specimen |
Abdominal Wall Transplantation
For patients with extensive abdominal wall defects after tumor resection and reduced abdominal cavity volume, the donor abdominal wall was transplanted as a free flap by the plastic surgeon, anastomosed to the recipient's inferior epigastric vascular system via microsurgery. Alternatively, if sufficient autologous skin was preserved, the donor abdominal fascia could be used directly for repair [Reddy et al., Ann Surg 2023].

Abdominal Wall Transplantation
Immunosuppression Regimen
• 500 mg methylprednisolone intravenously before reperfusion.
• 30 mg alemtuzumab intravenously after intraoperative reperfusion, with a second dose given 24 hours later.
• Tacrolimus for maintenance therapy, targeting trough levels of 10–12 ng/mL for the first six months, then reduced to 8–10 ng/mL.
• Since 2018, supplemental immunosuppression has included:
o Azathioprine (50–75 mg once daily).
o Mycophenolate mofetil (250–500 mg twice daily).
o Prednisolone (5–10 mg once daily).
Diagnosis and Treatment of Rejection
Small bowel rejection was diagnosed by endoscopy and biopsy, graded according to the criteria established by the 8th International Small Bowel Transplant Workshop. For patients who underwent abdominal wall transplantation, skin biopsies were performed if rash developed and assessed according to the 2007 Banff criteria.
Treatment of rejection included intravenous methylprednisolone for three consecutive days, along with adjustments to the immunosuppression regimen. Antithymocyte globulin was used additionally for persistent or severe rejection.
Bowel Transplant Failure
Bowel transplant failure was defined as any of the following after transplantation:
1. Resection of the transplanted bowel for any reason, including anastomotic leak, bleeding, ischemia, rejection, infection, malignancy, and graft-versus-host disease (GVHD).
2. Relisted for retransplantation.
3. Dependence on total parenteral nutrition (TPN):
o Restarting TPN after transplantation.
o Inability to discontinue TPN within three months of transplantation.
Results
With a median follow-up of 4.5 years, 6 patients died after transplantation. One patient died within 1 month post-transplant, two more (13%) died between 1 and 6 months post-transplant, and the remaining three (20%) died after 6 months post-transplant. Causes of death varied, including one death on postoperative day 24 due to anastomotic leak, one on postoperative day 69 due to upper gastrointestinal bleeding, and one on postoperative day 181 due to GVHD. Other causes of death included one patient who died on postoperative day 1001 after receiving palliative care for multiple complications, one on postoperative day 1204 due to disease progression, and one on postoperative day 1300 due to post-transplant lymphoproliferative disease.
Despite these challenges, most survivors achieved autonomous nutrition. Of the 14 patients who survived more than 1 month post-transplant, 12 successfully weaned off TPN, while the other 2 developed intestinal fistulas and remained on TPN. One year post-transplant, 72% (8/11) of patients no longer required home TPN support, but two later required home TPN supplementation due to post-transplant complications, including lymphoproliferative disease and pelvic tumor recurrence. Meanwhile, tumor progression or recurrence remained a significant challenge, affecting 91% of patients during at least 6 months of follow-up. The median time to recurrence was less than a year, at 363 days, ranging from 110 to 727 days [Reddy et al., Ann Surg 2023].
This study found that modified multi-visceral transplantation and small bowel transplantation are feasible for carefully selected patients with end-stage pseudomyxoma peritonei (PMP) who lack other surgical options. Follow-up results of the first patients receiving this treatment showed a 1-year survival rate of 78% and a 5-year survival rate of 55%, with a significant improvement in quality of life for the vast majority of patients. Key factors influencing surgical success include strict case selection, prioritizing patients with low-grade PMP, younger age, good health, and near-total tumor cell ablation, even in cases with high tumor burden, especially those with previous unsuccessful laparotomy.
Abdominal wall involvement presented a challenge for all patients, with nearly half (7/15) experiencing significant reduction in abdominal cavity volume due to tumor infiltration and tissue destruction. In these cases, primary anastomosis was not feasible due to excessive tension on the transplanted organs, increasing surgical risk. Despite these obstacles, survival outcomes remain promising. The 79% 1-year survival rate is comparable to global small bowel transplantation standards, while the 55% 5-year survival rate is slightly lower than the 60%-70% reported for non-PMP small bowel transplantation. However, these results are far superior to the prognosis of patients with unresectable PMP receiving only parenteral nutrition, who typically survive only 6-12 months. Notably, the 5-year survival rate of modified multi-visceral transplantation also surpasses that of mainstream cancer surgeries such as pancreaticoduodenectomy, highlighting its potential value as a treatment for this challenging disease [Reddy et al., Ann Surg 2023].
Although a high recurrence rate remains a challenge in transplantation treatment for PMP, careful patient selection and improving surgical expertise offer hope for improved outcomes. Transplantation has shown potential benefits for specific adenocarcinoma patients. Moreover, while tumor recurrence occurs under immunosuppression, most cases progress slowly. Notably, of the 15 deaths in this study, only 1 was directly attributed to tumor recurrence.
In 2021, Dr. Anil Vaidya in the US implemented a pioneering technique, introducing an innovative approach to multi-visceral transplantation. In this case, a combined liver and intestinal transplant was performed, along with a temporary splenic transplant to enhance immune protection and improve pancreatic blood supply. Additionally, a temporary right hemicolectomy was performed to help protect the newly transplanted bowel from infection and aid in nutrient absorption. After successfully fulfilling their temporary protective roles, the spleen and colon were subsequently removed.
Despite these advances, the small sample size and highly selected patient population of this study limit its generalizability. Several key questions remain unanswered, including the optimal timing of transplantation, the potential role of transplantation in treating higher-grade disease, and whether the addition of intraperitoneal hyperthermic chemotherapy at the time of tumor resection could improve disease control. Further research in this complex and evolving field of transplantation is crucial to refine patient selection criteria and explore methods to improve long-term survival rates.
In summary, small bowel transplantation is a feasible treatment option for selected patients with end-stage PMP, enabling long-term survival and improved quality of life. Further research is needed to refine patient selection criteria and explore adjuvant therapies to enhance efficacy.
转载自:
Key words:
Related News