Good Doctor. Hyperthermic Intraperitoneal Chemotherapy (HIPEC): Alternative to Traditional HIPEC - Three and Four Cycles of HIPEC
Intraperitoneal hyperthermic chemotherapy (IPHC) has remained largely unchanged in the past 30 years. It is used to prevent peritoneal metastasis in patients with a high risk of disease progression in gastric or colorectal cancer, and more commonly to treat patients with peritoneal metastasis from ovarian, gastric, colorectal, and appendiceal cancers. After undergoing cytoreductive surgery, IPHC is used to help maintain a disease-free state in the peritoneal and pelvic cavities. From a theoretical perspective and analysis of IPHC failures, this treatment method has several shortcomings. First, perhaps the most serious criticism of IPHC is its insufficient "dwell time" in the peritoneal and pelvic cavities. The chemotherapy solution is maintained at 41-43 degrees Celsius using a hyperthermia pump for only 90 minutes. This limited drug exposure time is even more problematic for residual micrometastases, as high intraperitoneal concentrations of most chemotherapeutic drugs are only maintained for 30-60 minutes. High-molecular-weight drugs like paclitaxel diffuse more slowly from the peritoneal cavity. Low-molecular-weight drugs like cisplatin no longer maintain high concentrations in the peritoneal cavity after only 20 minutes. My conclusion is that increasing the dwell time of chemotherapeutic drugs in the peritoneal cavity is the primary condition for achieving greater efficacy of IPHC.
2025-04-29
Triple and Quadruple Intraperitoneal Hyperthermic Chemotherapy
By Paul H. Sugarbaker
Intraperitoneal hyperthermic chemotherapy (HIPEC) has remained largely unchanged for the past 30 years. It is used to prevent peritoneal metastasis in patients with a high risk of disease progression in gastric or colorectal cancer, and more commonly to treat patients with peritoneal metastasis from ovarian, gastric, colorectal, and appendiceal cancers. After undergoing cytoreductive surgery, HIPEC is used to help maintain a tumor-free state in the peritoneal and pelvic cavities. From a theoretical perspective and analysis of failed HIPEC cases, this treatment method has several shortcomings. First, perhaps the most serious criticism of HIPEC is its insufficient "dwell time" in the peritoneal and pelvic cavities. The chemotherapy solution is maintained at 41-43 degrees Celsius using a hyperthermia pump, with an infusion time of only 90 minutes. For residual micrometastases, the limited drug contact time is even worse, as for most chemotherapeutic drugs, the high concentration of chemotherapeutic drugs in the peritoneal cavity can only be maintained for 30-60 minutes. High-molecular-weight drugs like paclitaxel diffuse more slowly from the peritoneal cavity. Low-molecular-weight drugs like cisplatin no longer maintain a high concentration in the peritoneal cavity after only 20 minutes. My conclusion is that increasing the dwell time of chemotherapeutic drugs in the peritoneal cavity is the primary condition for achieving greater efficacy of HIPEC.
In the past five years, an improved method of HIPEC has been published, namely multiple HIPEC after cytoreductive surgery, which can significantly prolong the dwell time of drugs in the body. Somewhat surprisingly, data on multiple HIPEC show that it is still effective even if cytoreductive surgery is not complete. I am skeptical about this. If a large number of lesions remain after surgery, resulting in most areas of the peritoneal cavity being unable to directly contact the chemotherapy solution, can this really improve patient survival? However, if adhesions and large lesions are removed, and the heated chemotherapy solution can reach most areas of the peritoneal and pelvic cavities, then a significant increase in the proportion of patients with significantly improved survival is expected in patients with peritoneal metastasis.
Clinical research and innovation in China have provided valuable information on the application of multiple HIPEC. In 2019, Yan Kangpeng's team from Nanchang, China, increased the dwell time of HIPEC after gastrectomy to four times the original time. Patients with peritoneal metastasis of gastric cancer underwent laparoscopic palliative gastrectomy, but no extensive cytoreductive surgery was performed. In the HIPEC group, an inflow catheter was placed in the upper and lower abdominal wall. The outflow catheter was placed in the hepatic diaphragm, splenic fossa, and pelvic cavity. The carrier solution was 2000 ml of saline. The chemotherapeutic drugs were oxaliplatin 150 mg plus 5-fluorouracil 1000 mg, the infusion temperature was 43 degrees Celsius, and the time for each HIPEC was 60 minutes. HIPEC was started on the first postoperative day and repeated on postoperative days 3, 5, and 7 (Yan K et al. JBUON, 2019).
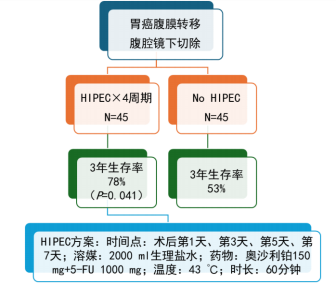
Figure 1. Efficacy of four cycles of postoperative oxaliplatin + 5-fluorouracil HIPEC in patients with peritoneal metastasis of gastric cancer undergoing laparoscopic resection.
After four cycles of HIPEC, Yan Kangpeng et al. reported that no major adjustments were needed for postoperative pain management, and there was no significant difference in the patients' physical functional status at postoperative and 3-month follow-up. At a median follow-up of 34.3 months, the 3-year survival rate for the 45 patients in the four-cycle HIPEC group was 78%, while the 3-year survival rate in the control group was 53% (p=0.041). There are currently no long-term follow-up data, and the paper does not clearly explain the specific grouping method for patients assigned to the simple laparoscopic gastrectomy group and the laparoscopic gastrectomy combined with four cycles of HIPEC group.
Lei Ziying's team presented data from the Chinese Peritoneal Tumor Study Group. They evaluated the use of three cycles of HIPEC for newly diagnosed stage III ovarian cancer patients. 2000 ml of saline containing 50 mg/m2 cisplatin was infused on postoperative days 1, 3, and 5, with the temperature set at 43 degrees Celsius and an infusion time of 60 minutes. This study used propensity score matching to analyze data from treated patients and historical controls. 423 patients received three cycles of HIPEC, while 159 patients did not receive HIPEC. The median survival time for patients receiving three cycles of HIPEC was 50 months, while the median survival time for patients not receiving HIPEC was 34 months (p<0.001). In addition, the 3-year survival rate for patients receiving three cycles of HIPEC was 60%, while the 3-year survival rate for patients not receiving HIPEC was 50% (p<0.001) (Lei et al. JAMA Open, 2020).
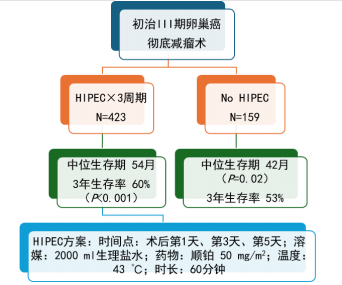
Figure 2. Evaluation of the efficacy of three cycles of cisplatin HIPEC after cytoreductive surgery in patients with stage III epithelial ovarian cancer.
For cholangiocarcinoma, intrahepatic bile ducts are often severely contaminated with cancer cells. Therefore, resection of cholangiocarcinoma is often accompanied by peritoneal metastasis. Feng Feiling's team in Shanghai, China, conducted a retrospective cohort study and published the results of a study on three cycles of HIPEC for patients with peritoneal metastasis of cholangiocarcinoma (Feng et al. Eur J Surg Oncol, 2021). Included patients underwent open resection of cholangiocarcinoma. 51 patients received three cycles of HIPEC and were compared with 61 patients who received only surgery. Three cycles of HIPEC were performed on postoperative days 2, 4, and 6. The intraperitoneal chemotherapy solution volume was 2 L/m2, the chemotherapeutic drugs were cisplatin 40 mg/m2 plus 5-fluorouracil 1000 mg/m2, the infusion temperature was 43 degrees Celsius, and the infusion time was 60 to 90 minutes. During HIPEC, pethidine hydrochloride and promethazine hydrochloride were given to relieve pain.
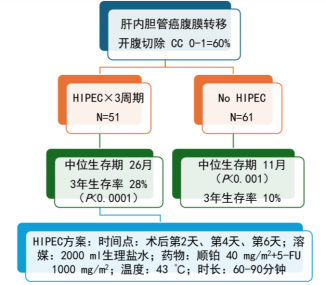
Figure 3. Evaluation of the efficacy of three cycles of HIPEC after cytoreductive surgery in patients with peritoneal metastasis of cholangiocarcinoma.
The following conclusions were drawn from the data provided in these three reports on the use of multiple intraperitoneal hyperthermic chemotherapy (HIPEC) after resection of abdominal or pelvic cancer. First, for these cancers with peritoneal metastases, a randomized controlled trial is necessary to confirm the benefits of multiple HIPEC. Second, and perhaps most importantly, the feasibility of performing multiple HIPEC outside the operating room has been demonstrated. Patients were able to receive intraperitoneal infusions of 2 liters of chemotherapeutic solution, tolerate a temperature of 43 degrees Celsius, and repeat treatments were feasible for highly motivated patients. Third, reasonable doses of chemotherapy were feasible. The dose of chemotherapy used was reduced by one-third to one-half compared to traditional single HIPEC. Finally, extending the drug dwell time of HIPEC to 3 to 4 times the original time was feasible, and these data suggest that multiple HIPEC offers greater benefits than traditional HIPEC.
Reprinted from:
Key words:
Related News


